About

Our Story
→
Experience seamless, enhanced diabetes monitoring and beyond with BUZUD CGM 2.0
Learn more
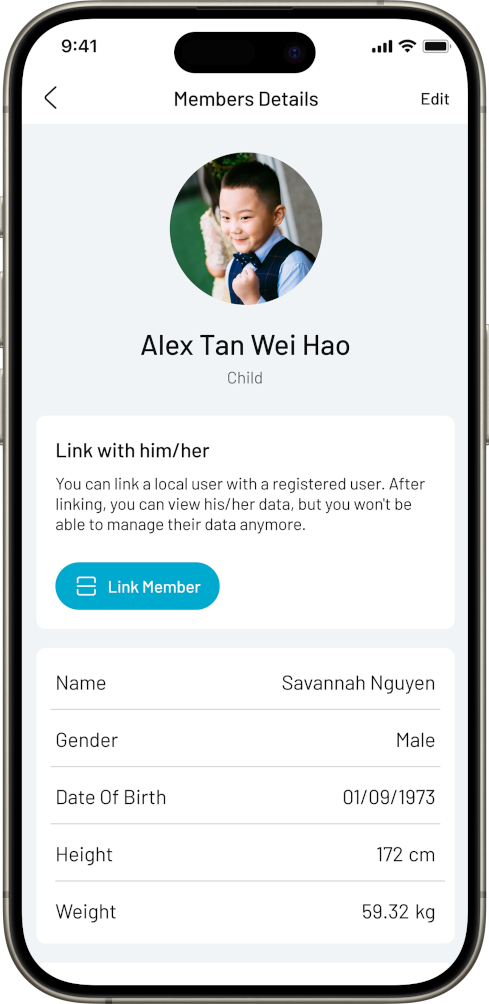
Take control of your health data anytime, anywhere. Manage your wellbeing with intelligent tools.



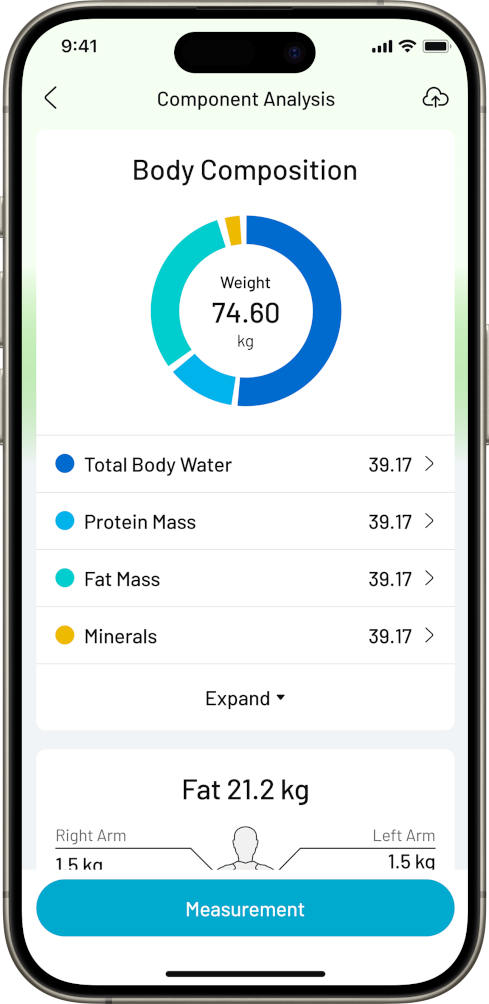

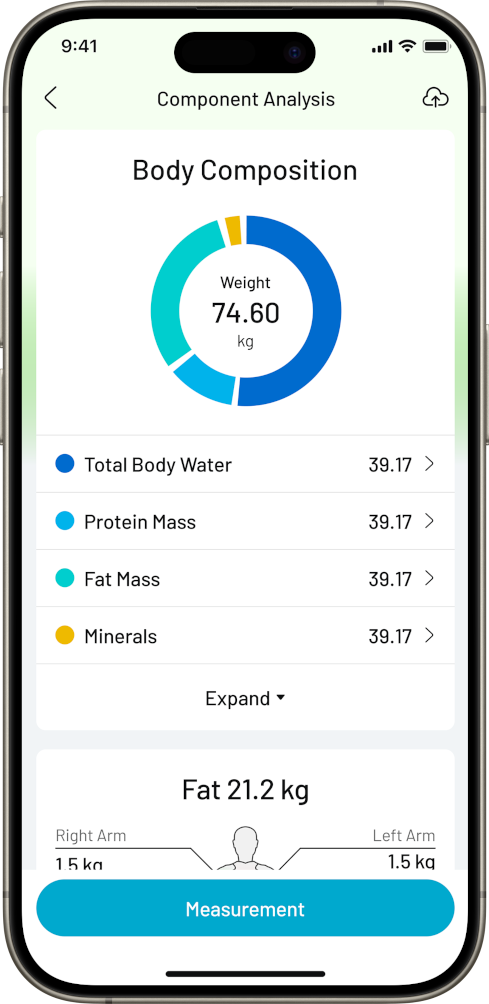


Integrating AI, data, and devices to deliver smarter, safer, and more personalized health solutions—for everyone.

AI recognizes food types and nutrients, and analyzes dietary impact by combining individual health data.

Machine learning evaluates medication effects and helps optimize dosage and timing for safer treatment.

Automatically detects exercise type and intensity, integrating real-time vitals for smarter fitness insights.

Deep learning interprets multi-dimensional health data to assist in early detection and clinical decisions.

BUZUD is committed to redefining healthcare through innovative technology and providing smart, reliable medical equipment and health management solutions to users around the world.
Continuous investment in R&D innovation to lead the development of medical technology
Strict quality management system to ensure product safety and reliability
Landing in the global market to serve users around the world
Focusing on user experience and providing humanized solutions
Learn about the latest developments of BUZUD
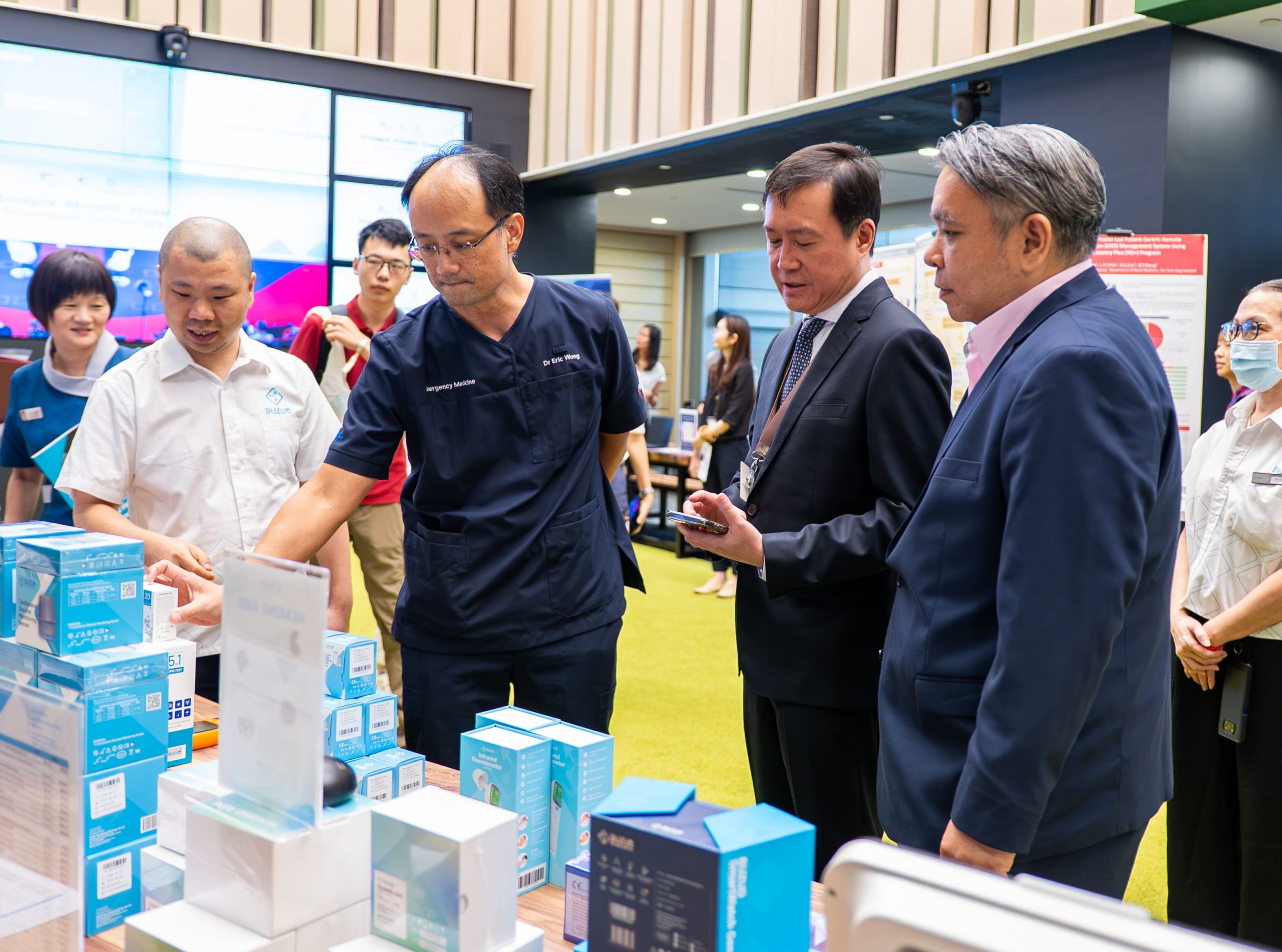
BUZUD, in collaboration with Tan Tock Seng Hospital (TTSH), has successfully introduced an innovative AI-powered mobile application paired with a wearable Continuous Glucose Monitoring (CGM) device. The solution, named CARB-CGM, was unveiled during a launch event on 26 February, marking a significant step forward in simplifying diabetes management and empowering patients to take control of their health. With diabetes projected to affect up to 1 million people in Singapore by 2050, this collaboration addresses the growing need for innovative tools to help patients manage their condition with greater confidence and convenience.
read more →
What a truly special day it was. At the International Medical University (IMU) in Malaysia, we did much more than sign an agreement — we celebrated a warm, meaningful milestone that feels like a big step forward in BUZUD’s story across Southeast Asia.
read more →Globally recognized certification, quality assurance
Health Sciences Authority of Singapore
U.S. Food and Drug Administration
EU medical device safety certification
Japanese Ministry of Health, Labor and Welfare certification
Australian Therapeutic Goods Administration certification
Certified by Health Canada
BUZUD products have obtained medical device certification in major markets around the world